Pose detection for online Achilles tendon rupture rehabilitation

Achilles tendon rupture (ATR) has become an increasingly common problem among adults in the last decades.
As the general population as well as athletes have returned to their normal routines after the COVID-19 crisis, the risk for injury (rupture, fracture) has increased after this enforced period of quarantines and lockdowns. Prior research has shown that returning to normal physical activity after periods of inactivity naturally causes more accidents.
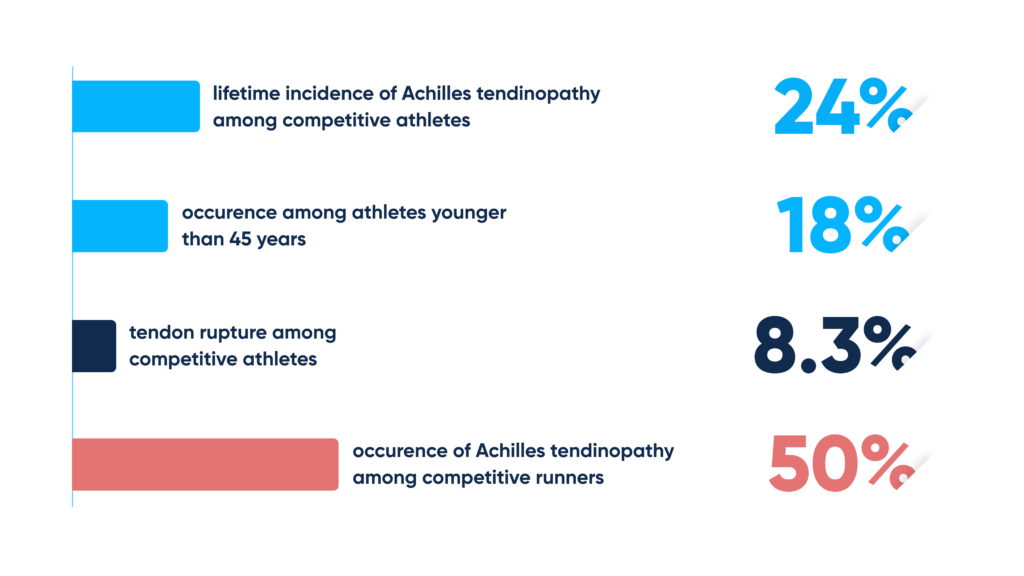
Achilles tendon rupture incidence
- Competitive athletes have a lifetime incidence of Achilles tendon rupture of 24%
- Competitive runners have a lifetime incidence of ATR of 40-50%
Achilles tendon rupture is sustained by competitive and recreational athletes, as well as the sedentary patient. It is typically accompanied by swelling and bruising, sudden pain, the inability to stand on toes, and difficulty while walking.
- The incidence of Achilles tendon rupture has increased in the past decades, mostly because of the rising popularity of situational recreational sports
- The incidence mostly occurs between 30 and 45, with a male-to-female ratio of 6:1
Achilles tendon rupture typically comes with substantial rehabilitation to regain muscle strength and mobility. The complexity of treatment usually depends on individual patient factors, injury severity, treatment method, the risk of complications, and defined long-term goals.
So, how is the musculoskeletal condition traditionally treated?
And what are the common limitations of conventional Achilles tendon rupture rehab?
ATR diagnosis – the methodology and opportunities
During the initial ATR diagnosis, the physician will inquire about symptoms, their onset, and how they progressed. Old injuries, as well as detailed social and medical history, are also very important (for example, athletic versus non-athletic patients may be treated differently due to potential re-rupture).
During the ATR examination, a patient with rupture may show significant weakness in ankle plantar flexion. Careful palpation may reveal tendon discontinuity or signs of bruising around the posterior ankle.
As stated in Clinical Sports Medicine, about 20% to 25% of Achilles tendon ruptures are misdiagnosed. Imaging tests (plain radiograph, ultrasound, MRI) might be ordered additionally to exclude other conditions, but are typically recommended in particular, ambiguous presentations and for preoperative planning due to their high labor intensity.
That is where introducing AI-based pose detection and analysis might drive sensibly better clinical outcomes. But more on rehab for Achilles tendon rupture recovery further below.
Achilles tendon rupture treatment: conservative methods, physical therapy, and rehabilitation
ATR treatment typically comprises:
- Conservative treatment, which involves local heat and cold, simple analgesics, as well as nonsteroidal anti-inflammatory agents to relieve the symptoms
- Physical therapy – gentle stretching, range-of-motion exercises, and deep heat modalities
Surgical intervention is usually only required for severe, persistent pain or progressive functional disability.
No matter the chosen treatment method (surgical, or nonsurgical), physical therapy and rehabilitation are critical. Recreational activities (walking, jogging, swimming, cycling) along with personalized exercises can improve muscle strength and range of motion.
The rehabilitation might differ based on the selected treatment approach and referring clinician’s protocols. This highlights the importance of accurate health assessment, correct diagnosis, treatment personalization, patient engagement, and continuous progress tracking.
ATR diagnosis – the limitations to overcome
Strain estimates during contraction of the calf muscles are obtained from voluntary tendon deformations. These are measured through B-mode ultrasound, which, however, isn’t always accurate enough, as the measurement outcomes are affected by so-called out-of-plane deformation due to tissue rotation or twisting. This problem is resolved using freehand 3D ultrasound, which integrates the B-mode ultrasound mentioned above. But still, this approach is limited by the tendon geometry.
Neuromusculoskeletal modeling, a method to estimate the internal tissue state, is another popular alternative. This approach has been shown to estimate physiologically plausible joint and tissue loading in various motion tasks but is highly labor-intense and is typically confined to the laboratory environment.
AI technology to facilitate ATR rehabilitation
Abto Software provides technology – camera-based markerless motion analysis for remote physical therapy – for high-quality human body motion recognition working seamlessly without additional physical equipment. The software is designed for remote physical therapy and rehabilitation and can be implemented to optimize Achilles tendon rupture treatment by providing value-added features enabling remote MSK therapy.
Watch the calf raises exercise captured by our human pose estimation technology:
Abto Software’s custom-designed technology – camera-based, real-time movement assessment and analysis – is meant to revolutionize human body motion capture to empower healthcare professionals as well as patients. Our solution might enhance Achilles tendon rupture recovery by enabling real-time feedback and guidance, progress tracking and visualization, and other advanced features ensuring immediate MSK benefits.
During sessions, the patient is guided virtually through a series of exercises – in this particular case, calf raises. While capturing, the technology automatically analyzes movement execution to evaluate overall performance and enable personalized adjustments.
But how can virtual physical therapy bring benefits to the healthcare provider?
And how does remote therapy monitoring outperform methods considered standard?
CV integration for efficient ATR recovery: the benefits
Accurate assessment
Pose detection can capture and evaluate the exercise by monitoring the positions of the hip, knee, ankle, and foot. This way, digital physical therapy ensures correct execution and facilitates patient outcomes.
Personalized care
Pose estimation can assist physical therapists in providing personalized care by considering individual needs. This way, remote physical therapy ensures the repetitions and range are tailored to the patient’s capabilities.
Real-time feedback and guidance
Utilizing AI motion tracking, healthcare providers can enable real-time feedback and guidance during sessions. By providing remote therapeutic monitoring (RTM), AI in physical therapy might enable timely interventions and minimize potential complications.
Progress tracking and visualization
By implementing AI physical therapy, healthcare professionals might leverage progress tracking and visualization. By reviewing and analyzing the repetitions, motion range, and endurance, telehealth in physical therapy enables value-added, patient-first care.
AI-empowered online rehabilitation: calf raises made convenient
Calf raises are a crucial element of the recovery regimen due to their efficiency in strengthening calf muscles. The loading of the Achilles tendon through this particular exercise is essential for regaining previous strength and flexibility.
AI-based markerless motion analysis can be successfully implemented to guide patients performing calf raises:
- Healing tissues – calf raises, if controlled and progressive, might accelerate the tendon healing process by stimulating its repair and remodeling through gradually increasing load
- Building strength – calf raises can target calf muscles, in particular, gastrocnemius and soleus muscles, which streamlines their strength
- Restoring functionality – this exercise helps regain ankle functionality, which enables normal walking and other everyday activities
- Preventing atrophy – this movement helps prevent and reverse muscle loss, which occurs after periods of immobilization
- Improving circulation – engaging muscles in the lower leg can also improve circulation and facilitate tissue repair and health
- Enhancing balance and stability – this exercise can enhance both balance and stability, thus preventing future injuries
AI enabling remote rehabilitation: potential applications
When damaged, the tendon loses strength and elasticity, negatively affecting the function of the lower leg. Through controlled physical therapy and rehabilitation, the tendon is gradually loaded, which stimulates a faster healing process by promoting blood flow and facilitating tissue regeneration.
AI-based markerless movement assessment can drive better outcomes by supporting patients performing:
- Toe-to-heel raises – gradually shifting body weight from toes to heels and back to strengthen both the foot and leg muscles
- Balance exercises – standing on one leg for at-home balance and stability training
- Calf stretches – by using a towel to pull the toes towards oneself, gently extending one leg to stretch calf muscles, and relieving Achilles tendon rupture symptoms
- Ankle dorsiflexion –gently stretching the tendon by moving one foot towards oneself (all exercises should be performed cautiously, especially after Achilles tendon rupture surgery)
- Leg lifts – lying on one side, lifting the top leg to strengthen hip abductors and support overall strength
- Partial squats – with feet hip-width apart, performing squatting without going too deep, to strengthen the quadriceps and glutes
How we can help
In the near future, Achilles tendon rupture rehab can be efficiently performed in ecologically valid settings, digitizing conventional physical therapy and rehabilitation.
AI-based pose detection, by eliminating excessive hardware and providing modern features, might optimize initial assessment, correct diagnosis, and treatment by facilitating greater precision, consistency, accessibility, real-time feedback and guidance, progress tracking and visualization, and other vital factors among others.
Our projects:
- AI-based jump recognition and analysis to improve public health
- CV-based human body pose detection to optimize physiotherapy monitoring
Our expertise:
- Artificial intelligence
- Computer vision
- Natural language processing (NLP)
- Optical character recognition (OCR)
Interested in implementing custom-built physical therapy exercise software?
Contact us to discover digital rehab!


